Influenza, commonly referred to as the flu, is an infectious disease caused by RNA viruses of the family Orthomyxoviridae (the influenza viruses), that affects birds and mammals. The most common symptoms of the disease are chills, fever, sore throat, muscle pains, severe headache, coughing, weakness/fatigue and general discomfort. Although it is often confused with other influenza-like illnesses, especially the common cold, influenza is a more severe disease than the common cold and is caused by a different type of virus. Influenza may produce nausea and vomiting, particularly in children, but these symptoms are more common in the unrelated gastroenteritis, which is sometimes, inaccurately, referred to as “stomach flu.” Flu can occasionally cause either direct viral pneumonia or secondary bacterial pneumonia.
Typically, influenza is transmitted through the air by coughs or sneezes, creating aerosols containing the virus. Influenza can also be transmitted by direct contact with bird droppings or nasal secretions, or through contact with contaminated surfaces. Airborne aerosols have been thought to cause most infections, although which means of transmission is most important is not absolutely clear Influenza viruses can be inactivated by sunlight, disinfectants and detergents. As the virus can be inactivated by soap, frequent hand washing reduces the risk of infection.
Influenza spreads around the world in seasonal epidemics, resulting in the deaths of between 250,000 and 500,000 people every year, up to millions in some pandemic years. On average 41,400 people died each year in the United States between 1979 and 2001 from influenza. In 2010 the Centers for Disease Control and Prevention (CDC) in the United States changed the way it reports the 30 year estimates for deaths. Now they are reported as a range from a low of about 3,300 deaths to a high of 49,000 per year.
Three influenza pandemics occurred in the 20th century and killed tens of millions of people, with each of these pandemics being caused by the appearance of a new strain of the virus in humans. Often, these new strains appear when an existing flu virus spreads to humans from other animal species, or when an existing human strain picks up new genes from a virus that usually infects birds or pigs. An avian strain named H5N1 raised the concern of a new influenza pandemic, after it emerged in Asia in the 1990s, but it has not evolved to a form that spreads easily between people.] In April 2009 a novel flu strain evolved that combined genes from human, pig, and bird flu, initially dubbed “swine flu” and also known as influenza A/H1N1, emerged in Mexico, the United States, and several other nations. The World Health Organization officially declared the outbreak to be a pandemic on June 11, 2009 (see 2009 flu pandemic). The WHO’s declaration of a pandemic level 6 was an indication of spread, not severity, the strain actually having a lower mortality rate than common flu outbreaks
Vaccinations against influenza are usually made available to people in developed countries. Farmed poultry is often vaccinated to avoid decimation of the flocks. The most common human vaccine is the trivalent influenza vaccine (TIV) that contains purified and inactivated antigens against three viral strains. Typically, this vaccine includes material from two influenza A virus subtypes and one influenza B virus strain. The TIV carries no risk of transmitting the disease, and it has very low reactivity. A vaccine formulated for one year may be ineffective in the following year, since the influenza virus evolves rapidly, and new strains quickly replace the older ones. Antiviral drugs can be used to treat influenza, with neuraminidase inhibitors (such as Tamiflu or Relenza) being particularly effective.
Classification
Types of virus
In virus classification influenza viruses are RNA viruses that make up three of the five genera of the family Orthomyxoviridae:
- Influenzavirus A
- Influenzavirus B
- Influenzavirus C
These viruses are only distantly related to the human parainfluenza viruses, which are RNA viruses belonging to the paramyxovirus family that are a common cause of respiratory infections in children such as croup, but can also cause a disease similar to influenza in adults.
Influenzavirus A
This genus has one species, influenza A virus. Wild aquatic birds are the natural hosts for a large variety of influenza A. Occasionally, viruses are transmitted to other species and may then cause devastating outbreaks in domestic poultry or give rise to human influenza pandemics. The type A viruses are the most virulent human pathogens among the three influenza types and cause the most severe disease. The influenza A virus can be subdivided into different serotypes based on the antibody response to these viruses. The serotypes that have been confirmed in humans, ordered by the number of known human pandemic deaths, are:
- H1N1, which caused Spanish Flu in 1918, and Swine Flu in 2009
- H2N2, which caused Asian Flu in 1957
- H3N2, which caused Hong Kong Flu in 1968
- H5N1, which caused Bird Flu in 2004
- H7N7, which has unusual zoonotic potential
- H1N2, endemic in humans, pigs and birds
- H9N2
- H7N2
- H7N3
- H10N7
Influenzavirus B
This genus has one species, influenza B virus. Influenza B almost exclusively infects humans and is less common than influenza A. The only other animals known to be susceptible to influenza B infection are the sea and the ferret. This type of influenza mutates at a rate 2–3 times slower than type A and consequently is less genetically diverse, with only one influenza B serotype. As a result of this lack of antigenic diversity, a degree of immunity to influenza B is usually acquired at an early age. However, influenza B mutates enough that lasting immunity is not possible.This reduced rate of antigenic change, combined with its limited host range (inhibiting cross species antigenic shift), ensures that pandemics of influenza B do not occur.
Influenzavirus C
This genus has one species, influenza C virus, which infects humans, dogs and pigs, sometimes causing both severe illness and local epidemics.However, influenza C is less common than the other types and usually only causes mild disease in children.
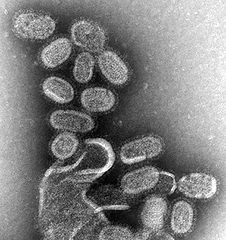
Structure, properties, and subtype nomenclature
Influenzaviruses A, B and C are very similar in overall structure. The virus particle is 80–120 nanometers in diameter and usually roughly spherical, although filamentous forms can occur.These filamentous forms are more common in influenza C, which can form cordlike structures up to 500 micrometers long on the surfaces of infected cells. However, despite these varied shapes, the viral particles of all influenza viruses are similar in composition. These are made of a viral envelope containing two main types of glycoproteins, wrapped around a central core. The central core contains the viral RNA genome and other viral proteins that package and protect this RNA. RNA tends to be single stranded but in special cases it is double. Unusually for a virus, its genome is not a single piece of nucleic acid; instead, it contains seven or eight pieces of segmented negative-sense RNA, each piece of RNA containing either one or two genes, which code for a gene product (protein). For example, the influenza A genome contains 11 genes on eight pieces of RNA, encoding for 11 proteins: hemagglutinin (HA), neuraminidase (NA), nucleoprotein (NP), M1, M2, NS1, NS2(NEP: nuclear export protein), PA, PB1 (polymerase basic 1), PB1-F2 and PB2.
Hemagglutinin (HA) and neuraminidase (NA) are the two large glycoproteins on the outside of the viral particles. HA is a lectin that mediates binding of the virus to target cells and entry of the viral genome into the target cell, while NA is involved in the release of progeny virus from infected cells, by cleaving sugars that bind the mature viral particles. Thus, these proteins are targets for antiviral drugs. Furthermore, they are antigens to which antibodies can be raised. Influenza A viruses are classified into subtypes based on antibody responses to HA and NA. These different types of HA and NA form the basis of the H and N distinctions in, for example, H5N1. There are 16 H and 9 N subtypes known, but only H 1, 2 and 3, and N 1 and 2 are commonly found in humans
Replication
Viruses can replicate only in living cells.Influenza infection and replication is a multi-step process: First, the virus has to bind to and enter the cell, then deliver its genome to a site where it can produce new copies of viral proteins and RNA, assemble these components into new viral particles, and, last, exit the host cell.
Influenza viruses bind through hemagglutinin onto sialic acid sugars on the surfaces of epithelial cells, typically in the nose, throat, and lungs of mammals, and intestines of birds (Stage 1 in infection figure). After the hemagglutinin is cleaved by a protease, the cell imports the virus by endocytosis.
Once inside the cell, the acidic conditions in the endosome cause two events to happen: First, part of the hemagglutinin protein fuses the viral envelope with the vacuole’s membrane, then the M2 ion channel allows protons to move through the viral envelope and acidify the core of the virus, which causes the core to dissemble and release the viral RNA and core proteins The viral RNA (vRNA) molecules, accessory proteins and RNA-dependent RNA polymerase are then released into the cytoplasm (Stage 2). The M2 ion channel is blocked by amantadine drugs, preventing infection
These core proteins and vRNA form a complex that is transported into the cell nucleus, where the RNA-dependent RNA polymerase begins transcribing complementary positive-sense vRNA (Steps 3a and b).The vRNA either is exported into the cytoplasm and translated (step 4) or remains in the nucleus. Newly synthesized viral proteins are either secreted through the Golgi apparatus onto the cell surface (in the case of neuraminidase and hemagglutinin, step 5b) or transported back into the nucleus to bind vRNA and form new viral genome particles (step 5a). Other viral proteins have multiple actions in the host cell, including degrading cellular mRNA and using the released nucleotides for vRNA synthesis and also inhibiting translation of host-cell mRNAs
Negative-sense vRNAs that form the genomes of future viruses, RNA-dependent RNA polymerase, and other viral proteins are assembled into a virion. Hemagglutinin and neuraminidase molecules cluster into a bulge in the cell membrane. The vRNA and viral core proteins leave the nucleus and enter this membrane protrusion (step 6). The mature virus buds off from the cell in a sphere of host phospholipid membrane, acquiring hemagglutinin and neuraminidase with this membrane coat (step 7) As before, the viruses adhere to the cell through hemagglutinin; the mature viruses detach once their neuraminidase has cleaved sialic acid residues from the host cell. Drugs that inhibit neuraminidase, such as oseltamivir, therefore, prevent the release of new infectious viruses and halt viral replication After the release of new influenza viruses, the host cell dies.
Because of the absence of RNA proofreading enzymes, the RNA-dependent RNA polymerase that copies the viral genome makes an error roughly every 10 thousand nucleotides, which is the approximate length of the influenza vRNA. Hence, the majority of newly manufactured influenza viruses are mutants; this causes antigenic drift, which is a slow change in the antigens on the viral surface over time. The separation of the genome into eight separate segments of vRNA allows mixing or reassortment of vRNAs if more than one type of influenza virus infects a single cell. The resulting rapid change in viral genetics produces antigenic shifts, which are sudden changes from one antigen to another. These sudden large changes allow the virus to infect new host species and quickly overcome protective immunity. This is important in the emergence of pandemics, as discussed below in the section on Epidemiology.